COVID-19 Day of Reflection
Date: 9 March 2025Today is COVID-19 Day of Reflection. A time to pause, remember, and reflect. We're sharing some of our staff and volunteers experiences during the pandemic.

“COVID-19 was a time of uncertainty across the country, and this was mirrored within the health service. What would we be dealing with; would we have enough people to support us? What risks would we be exposing our staff and volunteers to, and how would we work with a hybrid process for all our office functions.
“All these questions today seem so long ago, but at the time we didn't know what the future days, weeks and months and as we found out years, would look like. 
“What we did know however, was that our volunteers were offering support for activities and roles that they would not have normally been carrying out to support us with the unknown. The definition of a volunteer is 'a person who does something, especially helping other people, willingly and without being forced or paid to do it' (Cambridge Dictionary).
“We saw this nationally with the NHS volunteers, and locally with our community first responders. Not only did they want to continue to support their local community and respond to patients, they stepped up and got involved in providing community resilience to their local communities.
“Through those dark days, weeks and months we saw, felt and experienced the compassion, selflessness and generosity of our volunteers going above and beyond to support others.
“While we all have different experiences of COVID-19, either through the impact on our health and those close to us, or isolation and through the lockdowns we experienced, through it all I was humbled and proud of our volunteer workforce. They willingly supported us and asked us for additional ways they could help us and their communities.
Volunteers made COVID-19 more manageable for many people and for me will be the lasting memories of COVID19 - the positivity volunteering brought to many people’s lives, and how as a country we can all support each other.”
Lorna Hayes, Head of Community Response
 “Working as frontline clinician during the COVID-19 pandemic was a surreal experience. Like many other key workers, it was a strange paradigm to be unable to see your friends and family, yet spend 12-hour shifts working alongside colleagues, treating patients, having human contact yet enveloped in gowns, aprons, Tyvek suits, masks and respirators. Like everyone, the first few weeks and months of the pandemic were concerning with little known about what we were dealing with, what was safe, what was not and how dangerous this new virus really was.
“Working as frontline clinician during the COVID-19 pandemic was a surreal experience. Like many other key workers, it was a strange paradigm to be unable to see your friends and family, yet spend 12-hour shifts working alongside colleagues, treating patients, having human contact yet enveloped in gowns, aprons, Tyvek suits, masks and respirators. Like everyone, the first few weeks and months of the pandemic were concerning with little known about what we were dealing with, what was safe, what was not and how dangerous this new virus really was.
“It was a rapidly changing situation with every shift bringing new instructions, information and PPE. Of course, whilst all this was happening people continued to suffer with the usual medical emergencies. As a critical care paramedic on the East Anglian Air Ambulance at the time we saw a real change in the calls we received. With lockdown in full motion, we were called to fewer and fewer road traffic accidents, sporting injuries and trauma. Sadly, what we did see was a great increase in the number of cardiac arrest calls often in younger patients due to COVID-19.
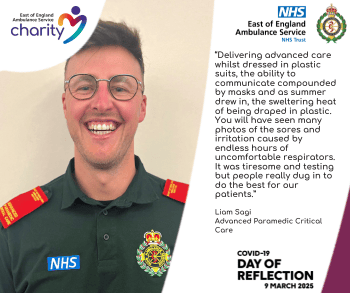
“Attending these calls was a new challenge for everyone. Delivering advanced care whilst dressed in plastic suits, the ability to communicate compounded by masks and as summer drew in, the sweltering heat of being draped in plastic. You will have seen many photos of the sores and irritation caused by endless hours of uncomfortable respirators. It was tiresome and testing but people really dug in to do the best for our patients.
“With so many intubated and ventilated patients, our skills on the air ambulance were drawn upon to support hospitals by transferring some the sickest patients between hospitals with capacity or indeed the newly formed Nightingale hospital. I was also undertaking extra ambulance shifts since so many staff were either off sick or isolating following a positive contact.
“The production of the vaccine felt like a huge sigh of relief for everyone – a glimmer of hope that we might start to be able to find out way out of this almost apocalyptic situation of empty streets, closed shops, absent community and excess mortality. I can only imagine how difficult it was for those who spent weeks and month at home alone, but this was crucial to prevent an even worse situation. I feel privileged to have been able to help during the COVID-19 pandemic despite all of this, but I hope we never have to face such a pandemic again.”
Liam Sagi, Advanced Paramedic Critical Care
 “I remember everything about the start of the COVID-19 pandemic because there was a lot that changed for me. If it hadn't of happened, I wouldn't have ended up at EEAST and working for the Ambulance Service or the NHS, it wasn't something that I had ever considered.
“I remember everything about the start of the COVID-19 pandemic because there was a lot that changed for me. If it hadn't of happened, I wouldn't have ended up at EEAST and working for the Ambulance Service or the NHS, it wasn't something that I had ever considered.
“I remember everything about the start of the COVID-19 pandemic because there was a lot that changed for me. If it hadn't of happened, I wouldn't have ended up at EEAST and working for the Ambulance Service or the NHS, it wasn't something that I had ever considered.
“I had got made redundant from an aviation role in January 2020. I found a new role in the hospitality industry which I started in the March. I knew something was wrong when I popped to the shops on the way home from one of my very first shifts and the shelves were bare. The hotel then closed, everyone was told to stay home, and I wasn't entitled to furlough.
“With a mortgage and responsibilities, I needed to be able to pay my bills. I saw on social media an advert for emergency call handlers. I had nothing to lose and met the criteria so I got straight onto the agency and had a telephone interview within days and started a few days after that at EEAST.
“Amongst the worry and unknown that everyone was going through, I felt a sense of security and responsibility. I felt proud that I was playing my part. I saw it then as more of 'digging in' and getting through whatever this was as opposed to seeing EEAST as what has turned out to be a flourishing career. My other half was luckily able to continue his key work and from the work/life balance point of view, there was a normality that many could only dream of.
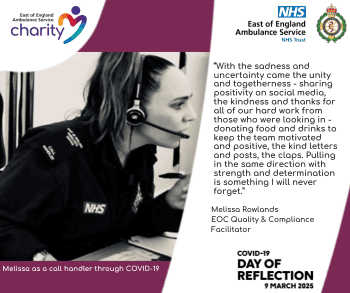
“With the sadness and uncertainty came the unity and togetherness - sharing positivity on social media, the kindness and thanks for all of our hard work from those who were looking in - donating food and drinks to keep the team motivated and positive, the kind letters and posts, the claps. Pulling in the same direction with strength and determination is something I will never forget.”
Melissa Rowlands, EOC Quality & Compliance Facilitator
 “At the time several colleagues in the area had to stand down for protective measures. Consequently, I became the sole active community first responder (CFR) covering North Bedfordshire from March to September 2020.
“At the time several colleagues in the area had to stand down for protective measures. Consequently, I became the sole active community first responder (CFR) covering North Bedfordshire from March to September 2020.
“This period coincided with my office closure and the transition to remote work, alongside my company's support of NHS pandemic efforts. This flexibility enabled me to dedicate additional hours to my CFR role, responding to 55 calls, including two cardiac arrests.
“While essential for personal safety, the mandatory full PPE requirement presented challenges. My glasses frequently fogged due to the mask, hindering visibility. Communication, particularly with elderly and hearing-impaired individuals, was also occasionally impeded.
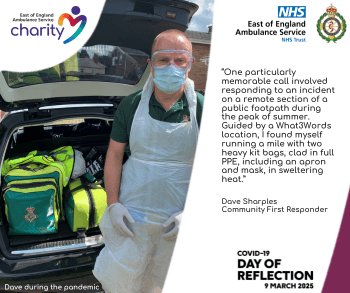
“One particularly memorable call involved responding to an incident on a remote section of a public footpath during the peak of summer. Guided by a What3Words location, I found myself running a mile with two heavy kit bags, clad in full PPE, including an apron and mask, in sweltering heat. I probably didn’t need to run but I didn’t know that at the time and it was a good workout!”
Dave Sharples, Community First Responder
“COVID-19 was a strange time. I qualified on 31 January 2020 only weeks before restrictions hit the world.
“I then remember as we went into lockdown, the disappointment at thinking of all of our frontline colleagues who had to go into battle because they were paid to, but as volunteers we were all stood down initially. I emailed a couple of staff I knew and assured them we were praying for them and had some lovely responses.
“Then in April 2020 we were allowed to respond again so I dutifully logged on duty but found that there were no alerts coming through - the number of calls had significantly been reduced. The public were avoiding adding any pressure to the NHS and so they were not phoning in. So, I clocked up hours and hours of duty but no calls. At least it meant that I got to complete my coursework for the CFR course (who remembers the course pack of work we had to write up within 6 months of the training).
“The same was true of June too although bit by bit we were allowed to go to more and more call types as the restrictions lifted. I can remember the first call after COVID-19 - the anxiety - would they have COVID-19 without knowing? Would I catch it from their doorhandle?
“In December the call volume went up significantly and we were responding to more and more calls.
“I remember going to an arrest during that time and being instructed by the crew on scene to get into the hazmat suits as they needed my help. There we were in a care home three floors up, working on the patient. I ran up and down that stairs in a hazmat suit at least twice to fetch more equipment. Even thought it was -5 degrees outside, it felt like it was about 35 degrees inside the hazmat suit.
“Then we went through 2021 when during the summer of 2021, the call volume was so high that it peaked high winter pressures - I can remember doing a 12 hour shift and being out of the house for 8 hours straight doing back to back calls.
“What a relief it was in 2021 to be able to scale back our PPE and stop wearing the aprons. Mind you I still have them in my kit and there are still jobs when I look at the information and think "do you know what, there is a chance this patient will vomit over me, so let’s apron and mask up".
There are some non-clinical things that stand out too - the call volume was so low that crews had more time to chat and I learnt more clinically during these times as crews had time to stop and teach me things about each patient. I built up a lot of friendships with the crews during this time and these connections are still going strong now.
“The friendship with crews is so strong that when I collapsed unexpectedly in the middle of the street two months ago, I was rushed to hospital semi-conscious. I don’t remember much about the first two hours of my time in hospital but I have learnt afterwards that it was all of these crews who were looking after me in hospital to ensure I got the best care - so thank you to all of the EEAST staff for everything you do - both what is seen and what is unseen.
“Together we will be the best ambulance service in the UK.”
Community First Responder
The NHS still needs support. If you'd like to help support your NHS heroes, you can donate to our East of England Ambulance Service Charity JustGiving Page.
